The terms we use
Language is a powerful tool. No single set of definitions can describe how every person experiences their health and wellbeing, or how they define themselves. We acknowledge the diversity of preferences and know that not everyone will agree with the terms we have chosen. It is always our intention to be inclusive and respectful.

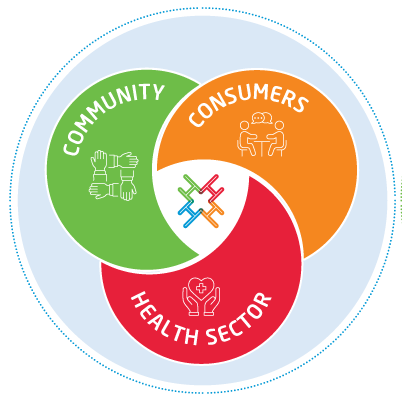
Consumers
People with lived and living
experience of health conditions, care,
harm and recovery including carers,
family members and supporters.

Community
People with an interest in improving
the health system, including
potential health service users
and volunteers.

Engagement
Working with consumers and
community members to listen,
collaborate, partner, inform and
create change.
Our values